OSTEOARTHRITIS
Be Aware, Scroll & Know OA Better

-
What is Osteoarthritis (OA)?
Do you know what osteoarthritis(OA) is?
This medical term is derived from:
Osteo = Bone; Arthritis = Inflammation in the Joint
It is one of the most commonly diagnosed arthritis. It can be called degenerative joint disease or “wear and tear” arthritis. Hands, hips and knees are usually affected. It is a myth that Arthritis is an old age problem. It is not a normal ageing process. In fact, arthritis is a chronic degenerative disorder involving cartilage damage.
The risk of getting this disorder is increased in older age groups but don’t think you are not at risk. You will be shocked to know that Arthritis has been diagnosed in the younger generation as well.
One in four adults will develop symptoms of hip OA by age 85.
One in two adults will develop symptoms of knee OA during their lives.
One in 12 people 60 or older have been diagnosed with OA.
More than 80 percent of people over age 55 show indications of OA on an X-ray.
-
TommusRhodus is an elite author known for offering high-quality, high-value products backed by timely and personable support. Recognised and awarded by Envato on multiple occasions for producing consistently outstanding products, it's no wonder over 40,000 customers enjoy using TommusRhodus themes.
-
How does it happen?
Osteoarthritis occurs when the cartilage (i.e. a protective Cushion at ends of bones) breaks down over a period of time. When the cushioning is damaged, there is no protection from friction. Even slight movement of the joint will lead to rubbing of the ends of bones together. The underlying bone begins to change its form. Certain chemical called cytokines get released. They cause inflammation, pain, stiffness and swelling. These develop slowly and worsen over time. Functioning of the joint reduces along with disability. The effects are so intense that some patients cannot even perform their day to day tasks.
-
TommusRhodus is an elite author known for offering high-quality, high-value products backed by timely and personable support. Recognised and awarded by Envato on multiple occasions for producing consistently outstanding products, it's no wonder over 40,000 customers enjoy using TommusRhodus themes.
-
Symptom Details
Affected joints might hurt during or after movement.
Joint stiffness maybe most noticeable in the morning or when inactive.
Applying light pressure causes the joint to feel tender.
- Loss of flexibility : Unable to move your joint through its full range of motion
- Grating sensation : You might feel a grating sensation when you use the joint and you might hear popping or crackling
- Bone spurs : Extra bits of bone, feeling like hard lumps, form around the affected joint, soft tissue inflammation around the joint causes local inflammation.
-
Risk factors
Factors that increase your risk of osteoarthritis include :
Old age : As the age increases the risk of having OA increases. It is commonly observed in the old age population.Risk increases with older age. Old age females are at higher risk compared to males
Weight : Joints like hips and knees experience stress due to increased weight, so if you are overweight you are at higher risk of developing OA. Fat tissue have the tendency to produce proteins which may lead to inflammation in and around your joints
Joint injuries : You can develop injuries from various sources like while playing sports or from an accident etc. These injuries might increase the risk of osteoarthritis.The injuries occurred few years ago that seems to have healed can also increase your risk of osteoarthritis
Repeated stress on the joint : The joint that experiences stress repetitively and regularly is at higher risk of developing OA
Genetics : Sometimes it is hereditary. Some people inherit a tendency to develop osteoarthritis
Bone deformities : Some people are born with malformed joints or defective cartilage
Certain metabolic diseases : People suffering from metabolic disorders like diabetes and hemochromatosis are at greater risk
Complications -
OA gradually worsens with time, leading to chronic pain. There is difficulty in performing daily tasks due to severe stiffness and pain in the joint. Pain and disabilities develop depression and disturbance in sleep.
-
How is OA Diagnosed?
The Orthopaedical physician or Rheumatologist diagnose OA based on the symptoms, physical examination, X-rays and lab tests.
-
IMAGING TESTS
The doctor may recommend you to get pictures of the affected joint.
X-rays : Cartilage is not seen in the X-ray images, but its loss is identified by the narrowing of the space between the bones in your joint. An X-ray also reveals the bone spurs around the joints
Magnetic resonance imaging (MRI) : MRI is used to develop a detailed image of bones and soft tissues, including cartilage. Generally MRI is not used for the diagnosis of OA, it is used in severe cases of OA to identify its complexity
-
LAB TESTS
Analysis of your blood or joint fluid will help to confirm the diagnosis.
Blood tests : There is no blood test for osteoarthritis, but certain tests help in identifying other causes of joint pain, e.g. Rheumatoid arthritis test
Joint fluid analysis : In this test doctor withdraws the fluid from your affected joint using a needle. Various tests are conducted from this fluid to determine the cause of your pain, i.e. whether the pain is due to gout or inflammation or infection rather than OA.
Your doctor might use a needle to draw fluid from an affected joint. The fluid is then tested for inflammation and to determine whether your pain is caused by gout or an infection rather than osteoarthritis.


Benefits of Exercise in OA
Makes you feel better by release of chemicals in your brain that reduce pain and boost your mood, such as serotonin
• Help you sleep better and give you more energy
• Loosen stiff joints and help keep them moving
• Strengthen and stretch muscles that help support and move your joints
• Improve overall fitness
• Make your heart and lungs stronger
• Help you get to and stay at a healthy weight
The Role of Physical Activity
One of the most beneficial things one can do to manage OA is to simply move. It may sound counterintuitive, especially when your body hurts, but moving is truly the best medicine for pain.
Unlike many diseases, exercise is considered as an option of treatment for OA – perhaps the most effective one. The American College of Rheumatology recommends exercise – particularly aquatic exercise – in its guidelines for treating knee and hip OA.
In fact, research shows that exercise may actually affect the course of OA. In a review of 28 studies of knee OA, exercise was found to be associated with an increased amount of cartilage within knee joints and fewer cartilage defects. Another study discovered a surge of anti-inflammatory activity within the knee joints of women with knee OA immediately after performing intense thigh strenghtening excercises.
You should, of course, discuss starting an exercise program withyour health care team. They can advise you on how to manage limitations and help create an easy-to-follow plan.
Try to incorporate the following three types of regular physical activity into your routine :
Stretching. Slow, gentle stretches, such as those that comprise yoga and tai chi, can help prevent joint stiffness and make it easier to get moving. These forms of exercise can improve flexibility, increase muscle strength and help you relax.
Aerobic activity. Engaging in regular physical activity is animportant part of controlling OAsymptoms. Aerobic exercise – any activity that gets your heart rate going – will strengthen your heart and lungs. Water exercises, walking and riding a stationary bicycle are less stressful on your joints than other aerobic activities.
Strengthening exercises. Activities that maintain and/or build strength and endurance in the muscles around affected joints are equally important. When muscles around a joint weaken,the joint loses its ability to function properly. The Arthritis Foundation offers land-based and water based exercise classes. For more information,contact your local office.
Flexibility and balance exercises. To help prevent falls, try to do gentle stretches or flexibility exercises every day. When doing muscle-strengthening exercises, you could mix in a few stretches; always stretch muscles while they are warm to reduce injury. Finally, add in exercises that help in increasing balance to help reduce the risk of falls.
How Much Activity Is Right for You?
- Two and a half hours (150 minutes) a week of moderate-intensity aerobic physical activity
- One hour and 15 minutes (75 minutes) a week of vigorous-intensity aerobic physical activity
- An equivalent combination of moderate and vigorous-intensity aerobic physical activity
- Aerobic activity should be performed in intervals of at least 10 minutes, preferably spread throughout the week
- Muscle-strengthening activities that involve all major muscle groups two or more days per week

Nutrition and Weight Loss
Another key tactic to managing OA is staying at your recommended healthy weight or losing weight if you are overweight or obese.
Benefits include:
- Preventing knee OA if not already diagnosed with.
- Easing pain by reducing stress on the weight bearing joints (hips, knees, back and feet).
- Enhancing overall feeling of well-being.
Unfortunately, there is no magic formula to help you lose weight. The basic rule for weight loss is eating in a calorie deficit and increasing physical activity. Your health care team can help you develop a safe,simple weight-loss program.
There is no “OA diet,” either, but in general you should eat a balanced diet which, according to the Food and Drug Administration, should be centered on plant-based foods. Approximately two-thirds of your diet should come from fruits, vegetables and whole grains. The other third should include fat-free or low-fat dairy products and lean sources of protein.

-
Go Fishing
CRP and IL-6 are proteins. When they go above normal levels, they cause inflammation in your body. Fish are rich in omega-3 fatty acids which fight inflammation, reduce C-reactive protein (CRP) and interleukin-6.
How much : At least 85-115 grams, two times in a week.
Best source : Salmon, tuna, sardines, anchovies and other cold-water fish.

-
Don’t Forget Your Fruits and Vegetables
Fruits and veggies are loaded with powerful antioxidants. They boost the immunity and help fight inflammation.
How much : At least 1½ to 2 cups of fruit and 2 to 3 cups of veggies per meal
Best source : Colourful foods such as cherries, strawberries, spinach, kale, broccoli, jamun

-
Eat a Handful of Nuts & Seeds
- Nuts consist of monounsaturated fats, protein and fibre. It fights inflammation and also helps in losing weight.
How much : Eat about a handful of nuts daily
Best source : Walnuts, pine nuts, pistachios, almonds

-
Boil the Beans
Legumes are known to have anti-oxidant and anti-inflammatory effect. You will get Fibre, protein, folic acid and minerals such as magnesium, iron, zinc and potassium which are very beneficial to us.
How much : At least one cup, twice a week
Best source : Try pinto, black, red kidney and garbanzo beans

-
Tablespoon of Extra Virgin Olive Oil
Olive oil contains Hydroxytyrosol and Oleocanthal among other polyphenols which are powerful anti-oxidants and have strong anti-inflammatory effect. It helps in reducing pain. It has been proven effective in improving symptoms in OA and RA
How much : Two to three tablespoons per day for cooking or 1 teaspoon in salad dressings or other dishes
Best source : Extra virgin olive oil is less refined and processed. Therefore, it retains more nutrients than standard variety of olive oil. Choose the oils packaged in dark bottles.

-
Cry on Some Onions
Onions are loaded with antioxidants. They may also reduce inflammation, heart disease risk and LDL, which is a bad cholesterol. Try them sautéed, grilled or raw in salads, stir-fries, whole-wheat pasta dishes or sandwiches.

-
Fill up on Fibre
Fibre lowers C-reactive protein (CRP) which is a substance in the blood that indicates inflammation. Getting fibre from diet lowers CRP levels more than popping fibre supplements.

-
Orange Red Food
The orange and red colour of carrots, peppers and other fruits is due to presence of anti-oxidant called Carotenoids. They are great in lowering CRP levels.
Best source : Carrots, red and yellow capsicum, apricot, cantaloupe (musk melon), mangoes, papaya, sweet potatoes, spinach, kale and pumpkin

FOOD TO AVOID

-
Don’t Sugar Up
Resisting sweets, chocolates, colas, milkshakes is a challenge for the mind. Sugar goes by many names so look out for any word ending in“ose,” e.g. fructose or sucrose on ingredient labels.

-
Cut Down On Saturated Fats
Mono-Saturated Fatty acids (MUFAs) are bad fats. Poly-Unsaturated Fatty Acid (PUFAs) are good Fats. MUFAs trigger fat tissue inflammation. It worsens arthritis and heart diseases. Read labels carefully before buying any product.
Resist the temptation to eat Pizza/ Cheese/ Red Meat/ pasta/ full-fat dairy products.

-
Avoid anything Processed
Trans fat can be found in fast foods, fried products, processed snack foods, frozen breakfast products, cookies, donuts, biscuits.
They trigger inflammation and are very harmful to the body.

-
No Omega 6 Fatty Acids
Omega 6 fatty acids are an essential fatty acid that the body needs for normal growth and development. The body needs a healthy balance of omega-6 and omega-3 fatty acids. Excess consumption of omega-6s can trigger the body to produce pro-inflammatory chemicals.
These fatty acids are found in oils such as corn, safflower, sunflower, grape seed, soy, peanut, and vegetable; mayonnaise and many salad dressings.

-
Refined Carbohydrates are White
White flour products (breads, rolls, crackers) white rice, white potatoes (instant mashed potatoes, or french fries) and many cereals are refined carbohydrates. According toScientific American, processed carbohydrates may trump fats as the main driver of escalating rates of obesity and other chronic conditions.
These high-glycemic index foods fuel the production of advanced glycation end (AGE) products that stimulate inflammation.

-
MSG in your Chinese
Mono-sodium glutamate (MSG) is a flavour-enhancing food additive. This chemical can trigger two important pathways of chronic inflammation and affect liver health.
It is most commonly found in prepared Asian food and soy sauce but it can also be added to fast foods, prepared soups and soup mixes, salad dressings and deli meats.

-
Don’t go Sugar-Free
Trying to be healthy and go sugar-free?
Aspartame is a non-nutritive, intense artificial sweetener found in more than 4,000 products worldwide.
It may trigger an inflammatory response in some people.

-
Say No to Alcohol
Alcohol is a burden to the liver. Excessive use weakens liver function and disrupts other multi-organ interactions and can cause inflammation.
It is best eliminated or used in moderation.

-
-
Salt a.k.a Sodium
Read labels carefully. Salt by any other name is still salt. Look for salt’s alias – sodium. Look for products labelled sodium-free, salt-free, low-sodium, very low-sodium, reduced or less sodium or light in sodium.
Try a salt substitute.
Give vegetables a good rinse. Washing thoroughly in cold water can reduce their salt content by almost half.
Use herbs and spices instead of salt to season foods. Pepper, lemon juice and vinegar can all enhance flavour.
Switch from packaged cereal or packets of instant oatmeal to quick-cut oats.
Fresh meats, fruits and vegetables and whole grains are naturally low in sodium.
Eat home-made food.
Products such as ketchup, mustard, pickles, olives, sauerkraut, Worcestershire sauce or soy sauce are almost always high in sodium.
Tell someone to hide the snacks so that you can`t reach it.
-
Management Of
the design conscious
Assistive Devices
Assistive devices are often used by people whose pain or instability limits physical activity, who are not eligible for surgery, who do not wish to undergo surgery or to delay it. These tools can help to decrease pain and improve ability to move.
The tools may include supports, braces, splints and shoe orthotics as well as canes and walkers, which help support joints and/or provide rest to the joint while you go about your everyday activities.

Physical and Occupational Therapy
You may find that OA limits certain activities, such as walking, bathing, dressing, climbing stairs and doing household chores. Physical and occupational therapists can help improve your ability to perform these activities and help you manage OA by designing a program that may include :
- Improving your joint range-of-motion muscle strength and endurance
- Providing and fitting assistive devices to make daily activities easier
- Showing you how to use heat therapy and cold therapy – applying simple heat packs or cold packs to relieve pain
- Education regarding principles of proper joint use and energy conservation

The Four-Pound Rule
Research has shown that every excess pound places an extra four pounds of pressure on your knees, so losing even a few pounds can make a significant difference in prevention of OA.

Pain Management
Controlling pain is the hardest part of managing OA.
Pain creates a vicious circle of inactivity, which leads to greater pain, and thus greater inactivity.
However, studies show most people note improvement in their OA symptoms with physical activity, physical therapy or occupational
therapy, or the other techniques just discussed.
Medication can also help you control pain enough to start an exercise program.
Your doctor will work with you to decide what’s best for you.
Non-Opioid and Opioid Analgesics
Analgesics are medications used for pain relief. Acetaminophen (Tylenol) is a non-opioid (ornon-narcotic) analgesic often used for pain relief. It doesn’t reduce the inflammation or swellingsometimes associated with OA, but it is helpful when pain is the main problem and can be safer than other medications used to treat OA.
While the number of potential side effects due to acetaminophen are small, there is a risk of liver damage or failure when taking high doses. Do not take more than 4,000(mg) total per day.
NSAIDs (Pain Killers)
Nonsteroidal anti-inflammatory drugs, or NSAIDs, help reduce joint pain, stiffness and swelling. Aspirin, ibuprofen and naproxen sodium are examples of NSAIDs that are available over the counter. Oral and topical prescription NSAIDs are also available to treat OA. Oral NSAIDs can cause side effects such as pain or bleeding in the stomach. If you experience these side effects or have an increased risk for a stomach ulcer or bleeding, your doctor may prescribe other medications that may help reduce the risk of these problems.
Nutritional Supplements
Glucosamine and chondroitin sulfate are nutritional supplements derived from cartilage, are believed to offer relief from OA pain by many people.
Topical Pain Relievers
Topical pain relievers are available as creams, gels, patches, rubs, drops or sprays that are applied on the skin over a painful joint. They may contain combinations of salicylates, skin irritants and local anaesthetics to relieve pain.
Injectables
Joint injections are often used by people with OA. Often, injections straight into the joint can help with symptoms without some of the side effects that other treatments may have.
Non-Medicinal Pain Relief
In addition to staying active and losing weight, you can fight OA pain with some tried-and-tested remedies, including:
Hot and cold treatments: Usually applied directly to the pain site, heat may be more useful for chronic pain; cold packs may provide relief from acute pain. Bags of frozen vegetables, such as peas, make excellent, easily mouldable cold packs.
Relaxation techniques: Techniques such as deep breathing, guided meditations and visualization, help in relaxing the mind and reducing stress.
Massage. Research shows massages can help ease arthritis pain, improve joint function and ease stress and anxiety.
Acupuncture: Acupuncture, the practice of inserting fine needles into the body along special points called “meridians,” has been shown to relieve and control pain.
Positive attitude: Many studies have demonstrated that a positive outlook can bolster the immune system and increase the ability to handle pain.

-
-
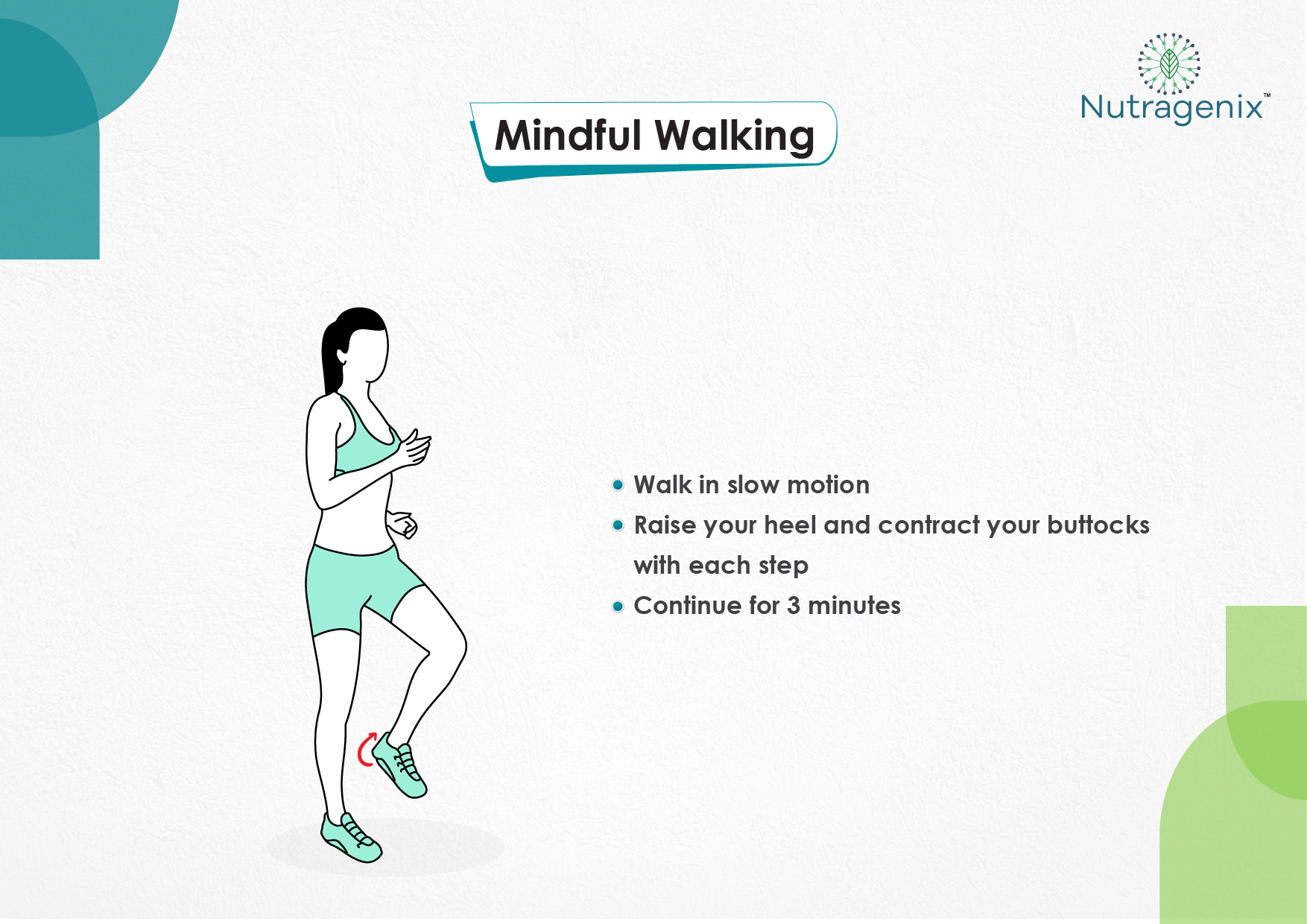
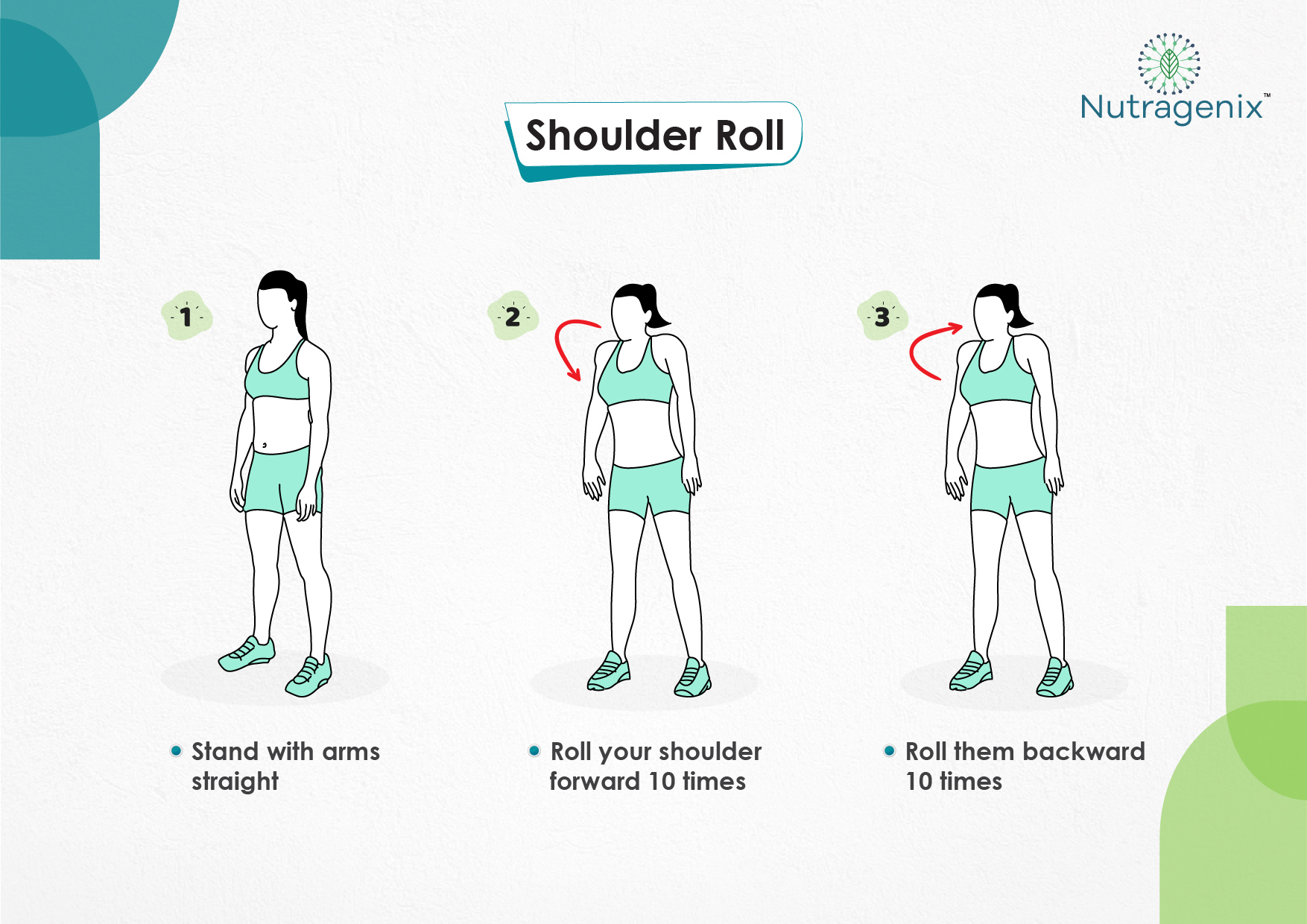
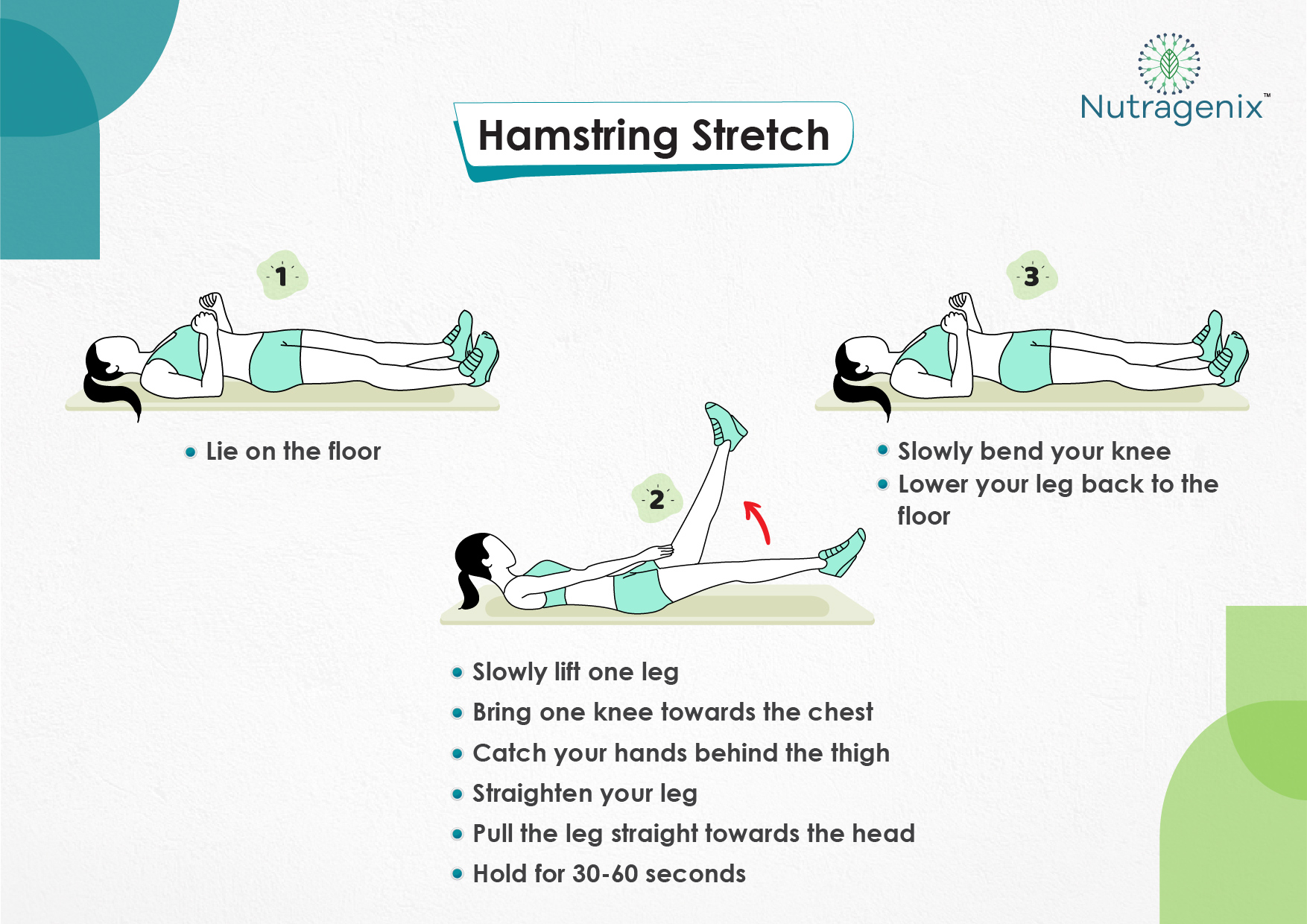
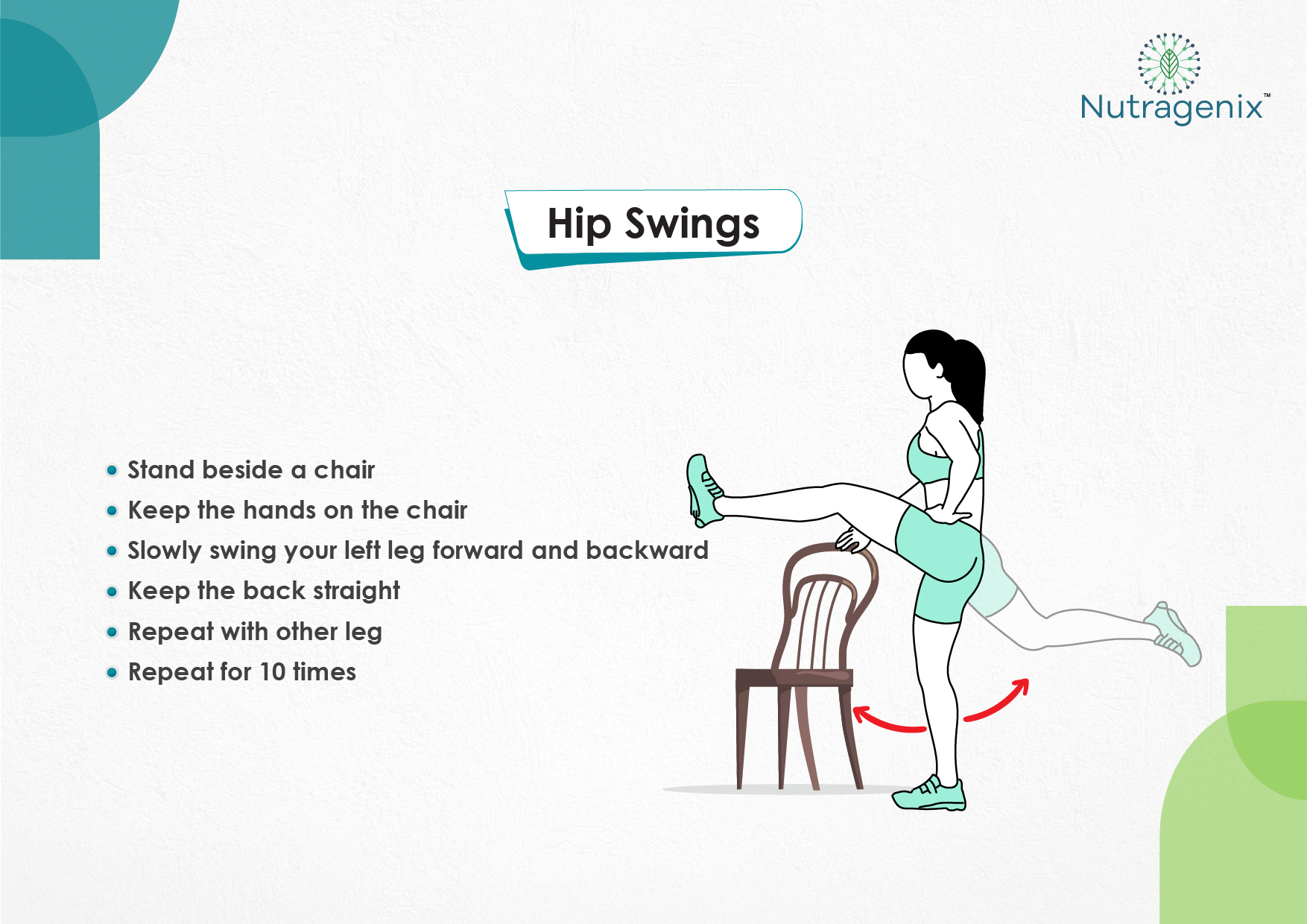
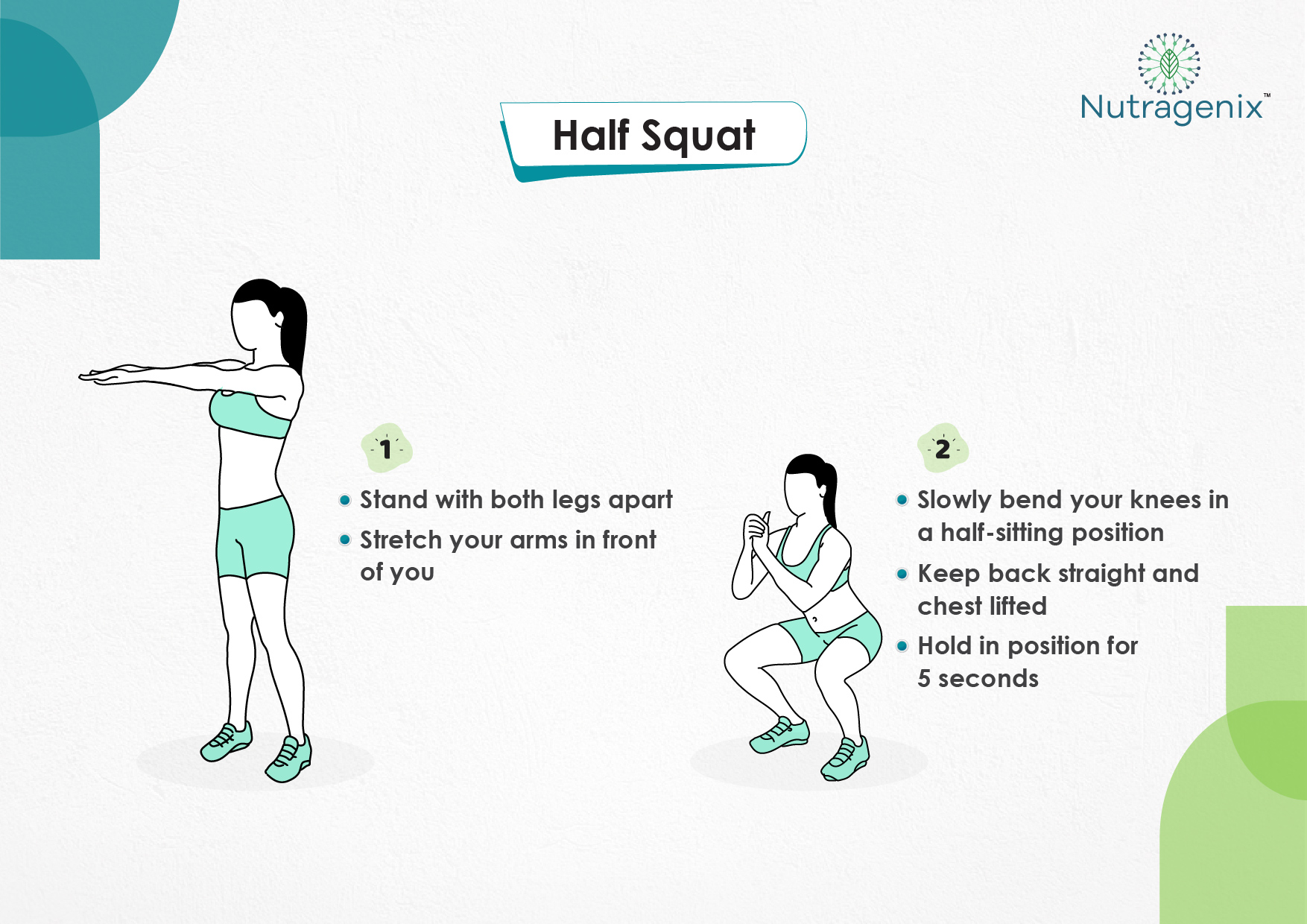
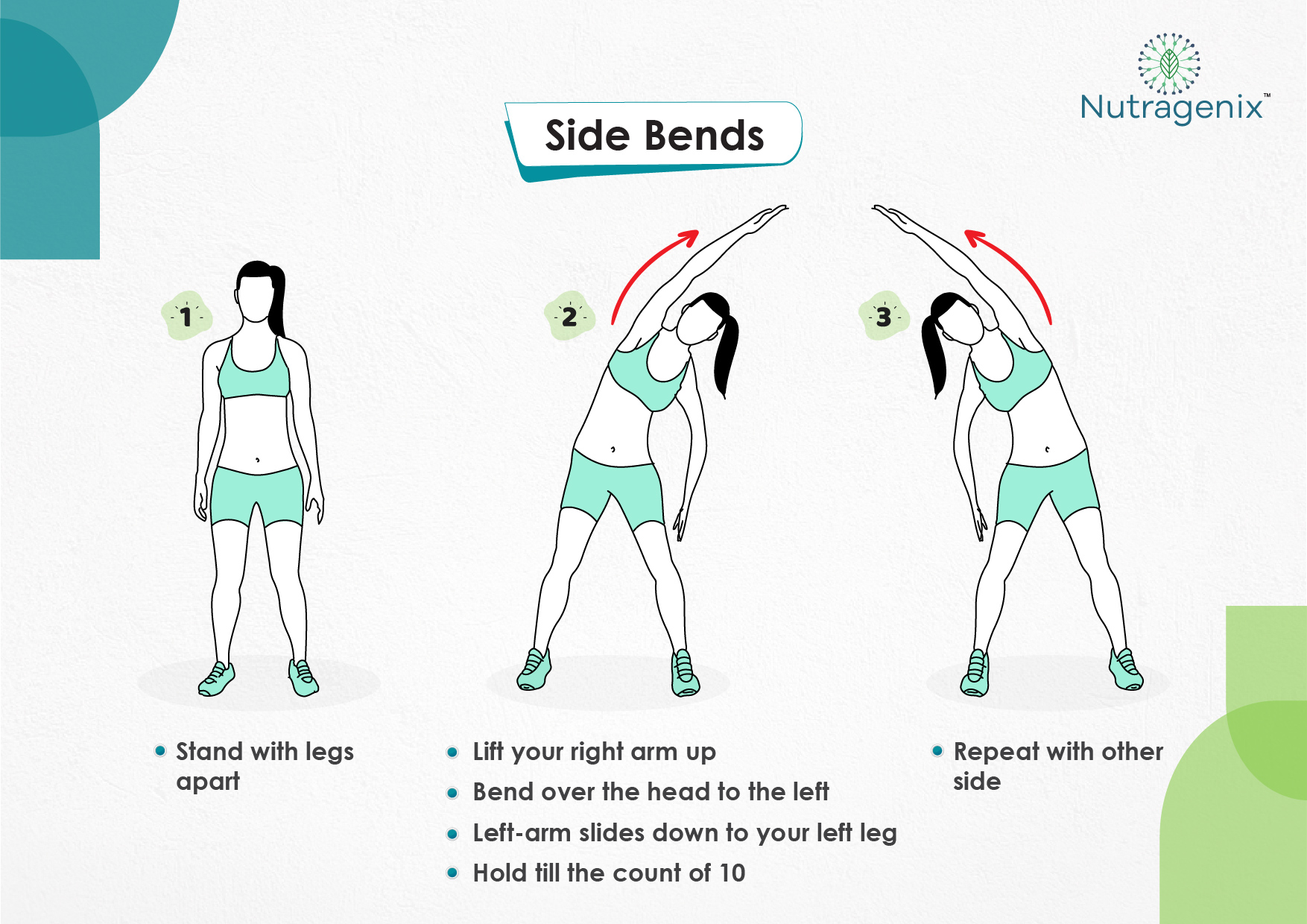
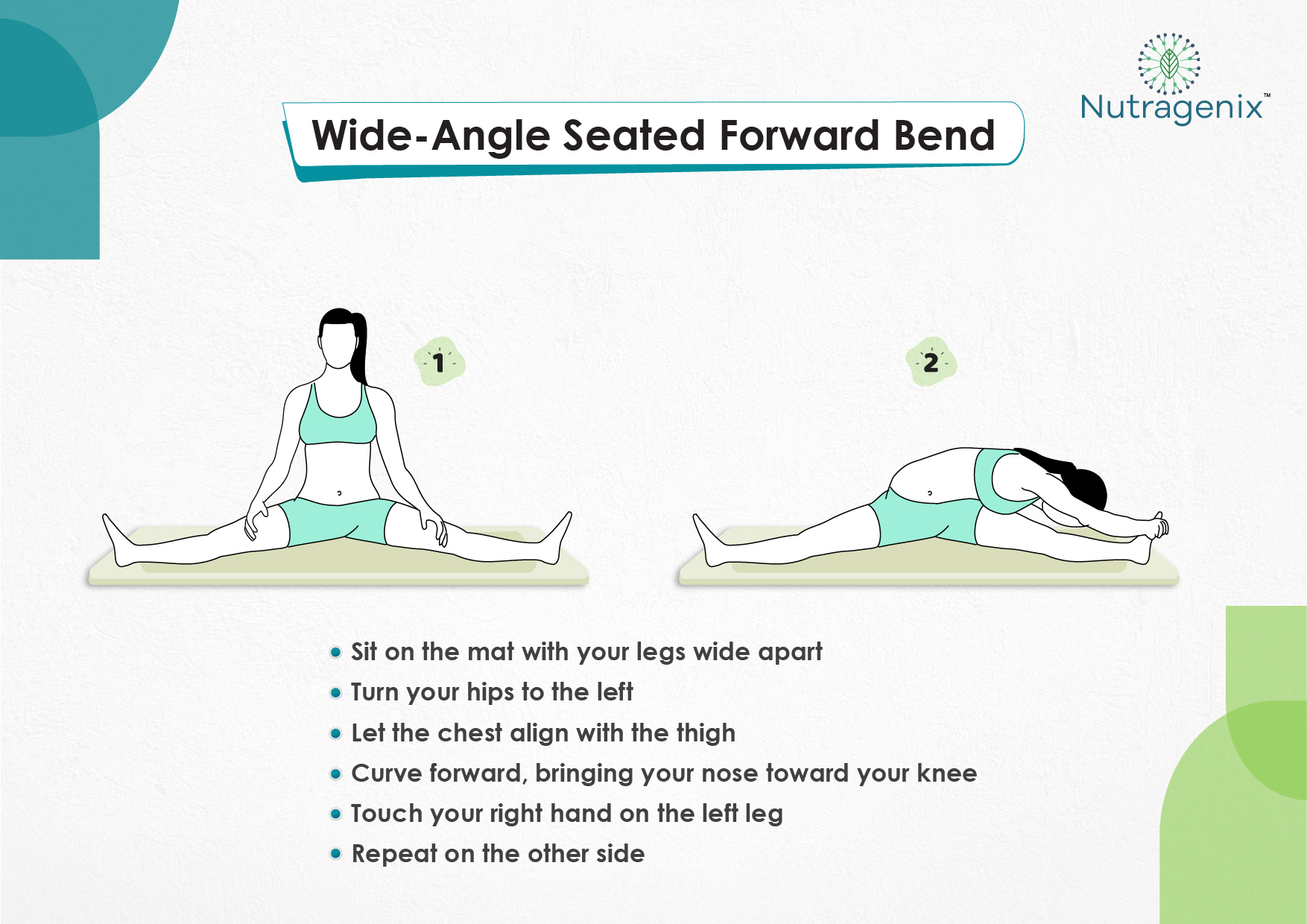
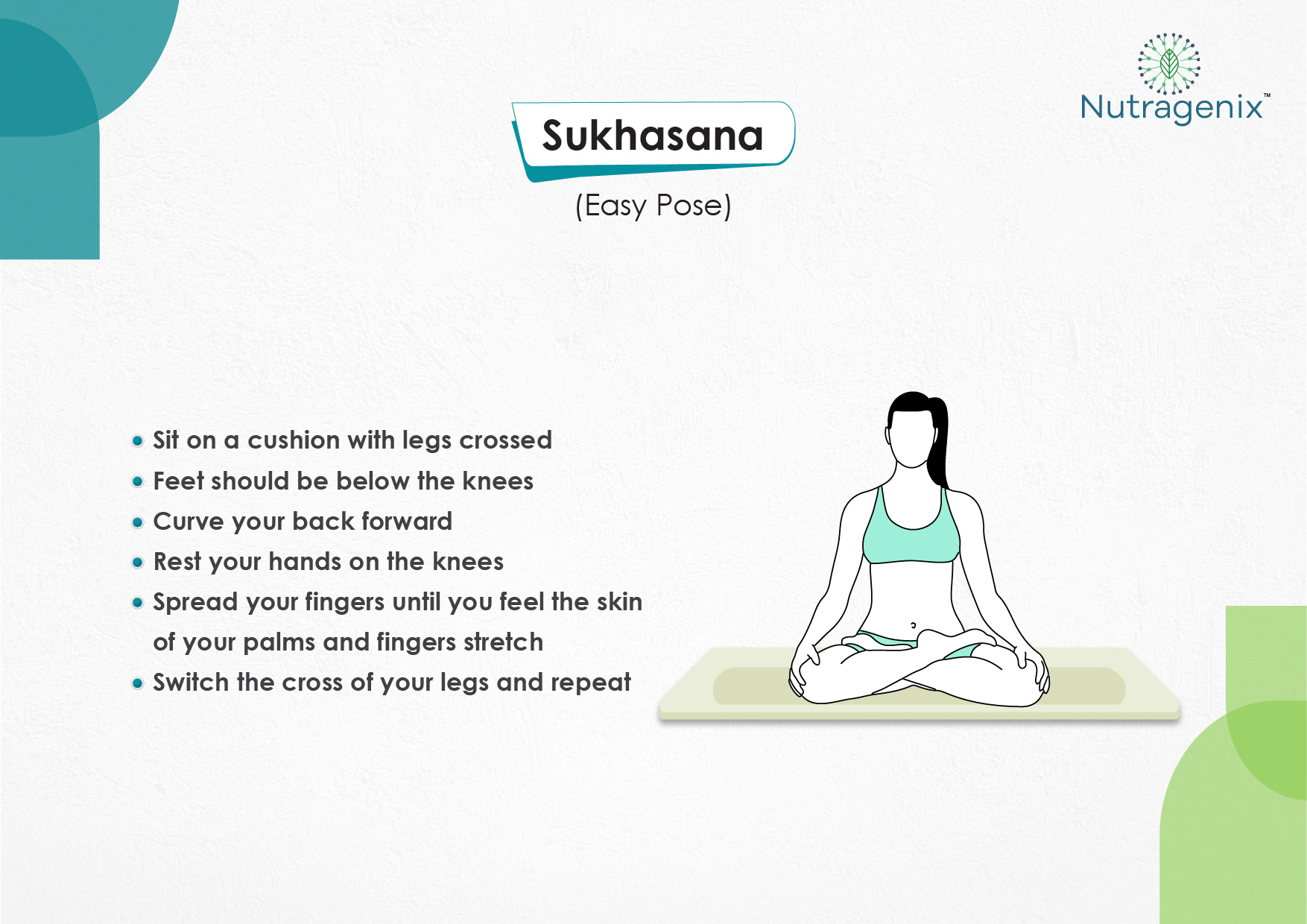
Knee and Hip Exercises for Osteoarthritis
If you have osteoarthritis (OA) in your hips or knees, exercising may be the last thing you feel like doing. Symptoms like pain and stiffness in your joints can make it tough to work out. But moving is important for hip and knee OA. It causes your joints to compress and release, bringing blood flow, nutrients, and oxygen into the cartilage. Physical activitycan also help you feel better.
-
-
“Along with boosting your overall health, exercise can improve your OA symptoms like pain, stiffness, fatigue, and even depression", says Leigh F. Callahan, PhD, associate director of the University of North Carolina Thurston Arthritis Research Center.
-
One study found that people with knee OA who worked out regularly lowered their pain by 12% compared to those who didn’t.
Ready to lace up your sneakers?
No single workout is best but some moves are better for hip and knee OA. Experts recommend doing a mix of the following three exercises. But first, remember to check in with your doctor before you start any new physical activity.
-
Aerobic exercise
This is the type that strengthens your heart and helps your lungs work better. “It also burns calories, which can help you lose or maintain a healthy weight,” Callahan says. That’s important, because extra pounds add stress onto your hip and knee joints.
If you’re new to exercise, start with low-impact activities. They’re gentle on the joints. Good options for hip and knee OA include:
-
- Walking
- Swimming
- Biking
- Elliptical training
- Cross-country skiing
To ease the pain and lower your odds of an injury, don’t try to do too much at once. “Start with just 10 minutes,” says Arina Garg, MD, a rheumatology fellow at The Center for Excellence for Arthritis and Rheumatology at the Louisiana University Health Sciences Center. “Every few days, increase that time by 5 to 10 minutes.” Your goal is to work up to 30 minutes of aerobic exercise, 5 days a week.
-
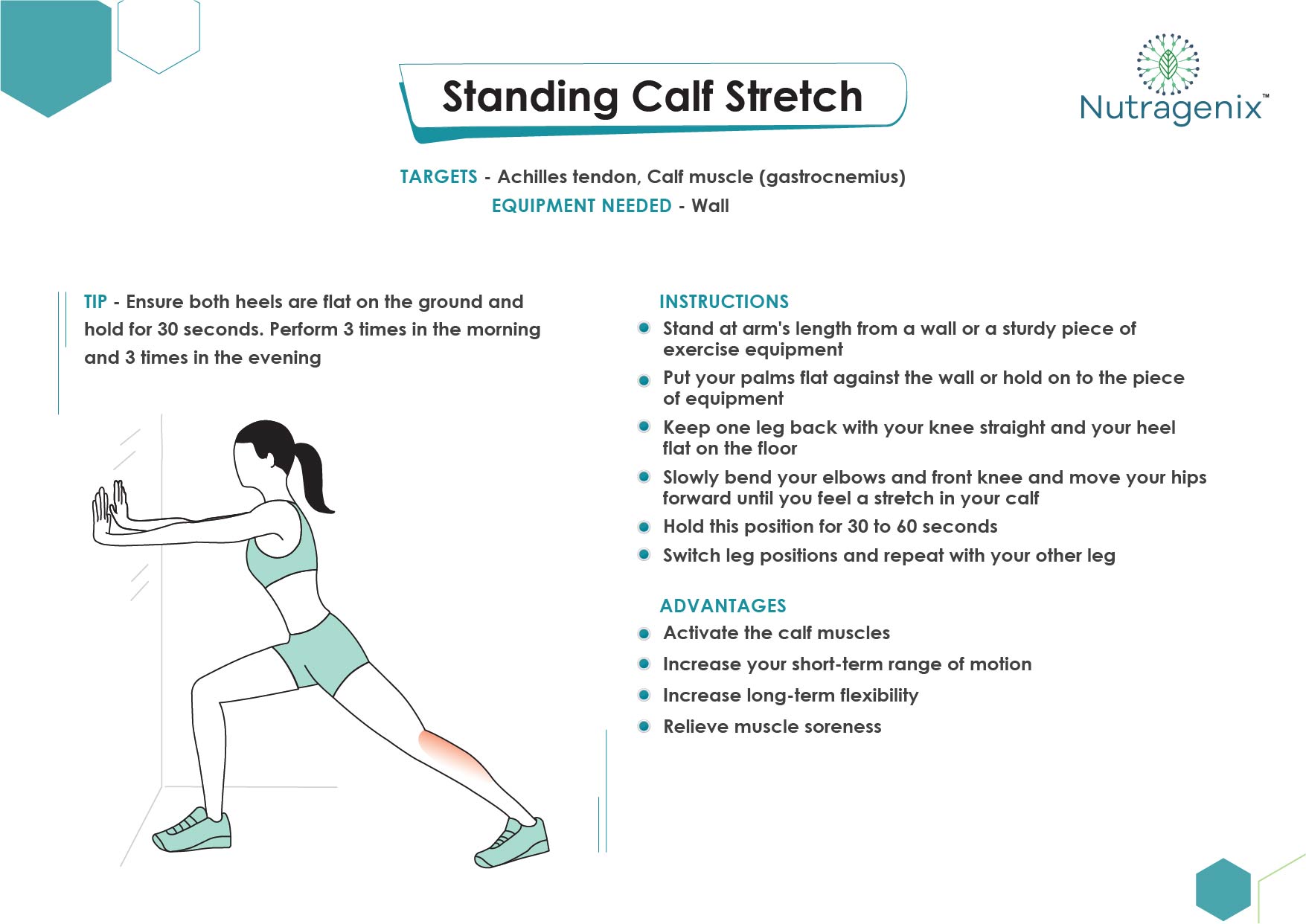
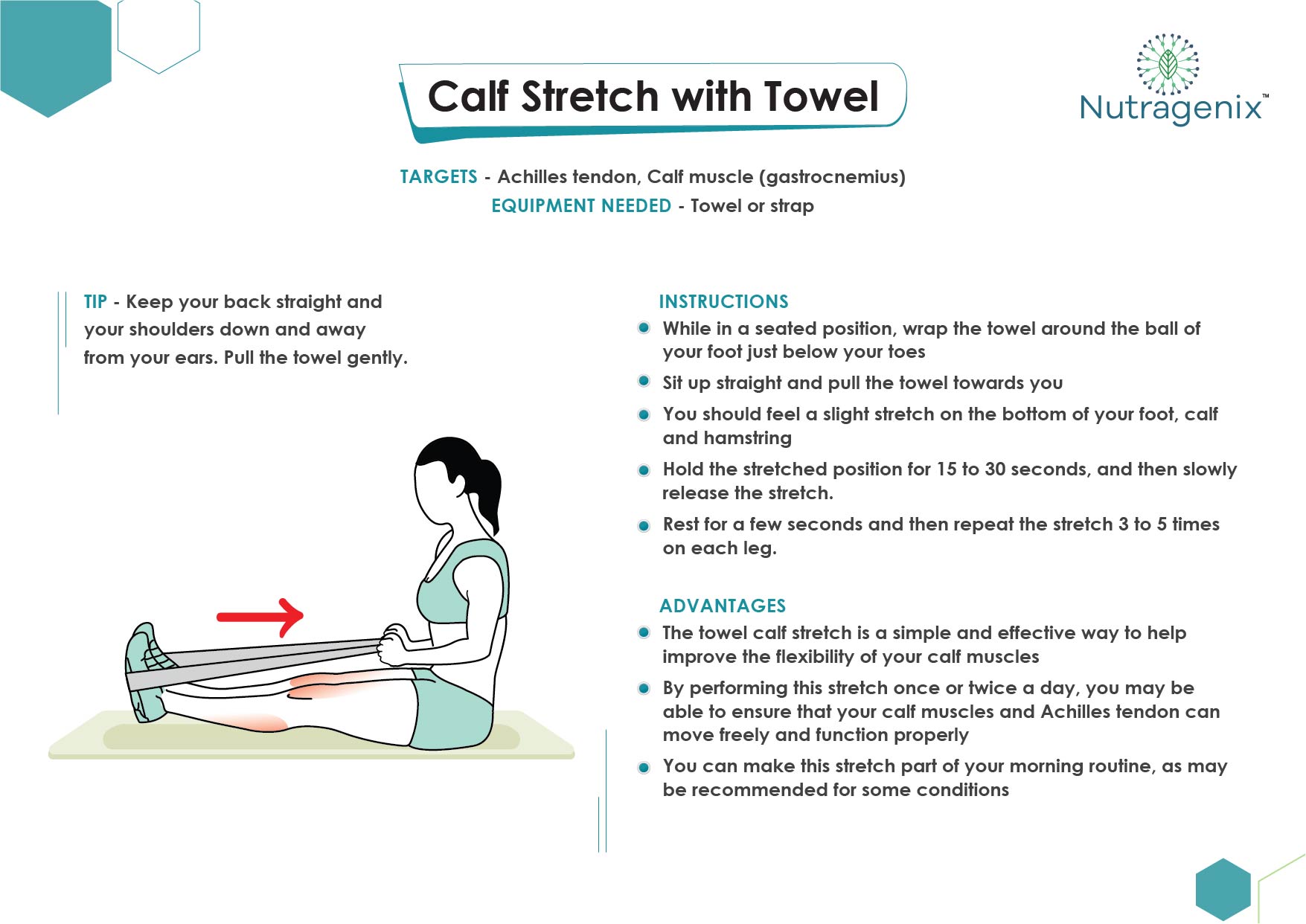
Flexibility (range-of-motion) exercises
The first step is flexibility exercise to improve joint mobility, reduce stiffness and help prevent tightening of the tissues around the joint.
Flexibility exercises gently stretch and lengthen the muscles and move the joints through a range of motion that's comfortable — you should not feel pain — but produce a sensation of resistance. You should perform these exercises (see examples) when you are feeling the least pain and stiffness — for example, after a warm shower or at the end of the day. If you take a pain reliever, do your stretching when the drug is having its strongest effect. You can start with just one or two exercise a day, three times a week, but try to work up to performing several, at least once a day.
-
Strength (resistance) training
By strengthening muscles, you protect and support affected joints and improve overall function. Inactivity due to osteoarthritis, as well as aging in general, can reduce muscle mass, contributing to frailty and weakness.
Strength training involves contracting the muscles against resistance. The resistance can be from your own body or from hand or ankle weights or resistance bands. Your clinician will recommend specific exercises based on the condition of your joints and your level of pain. Muscles should not be exercised to the point of fatigue. Start with four to six repetitions rather than the eight to 12 normally associated with resistance training. If you have joint pain that lasts more than an hour after you exercise, you're probably overdoing it. You should not do strength training more than two days per week.
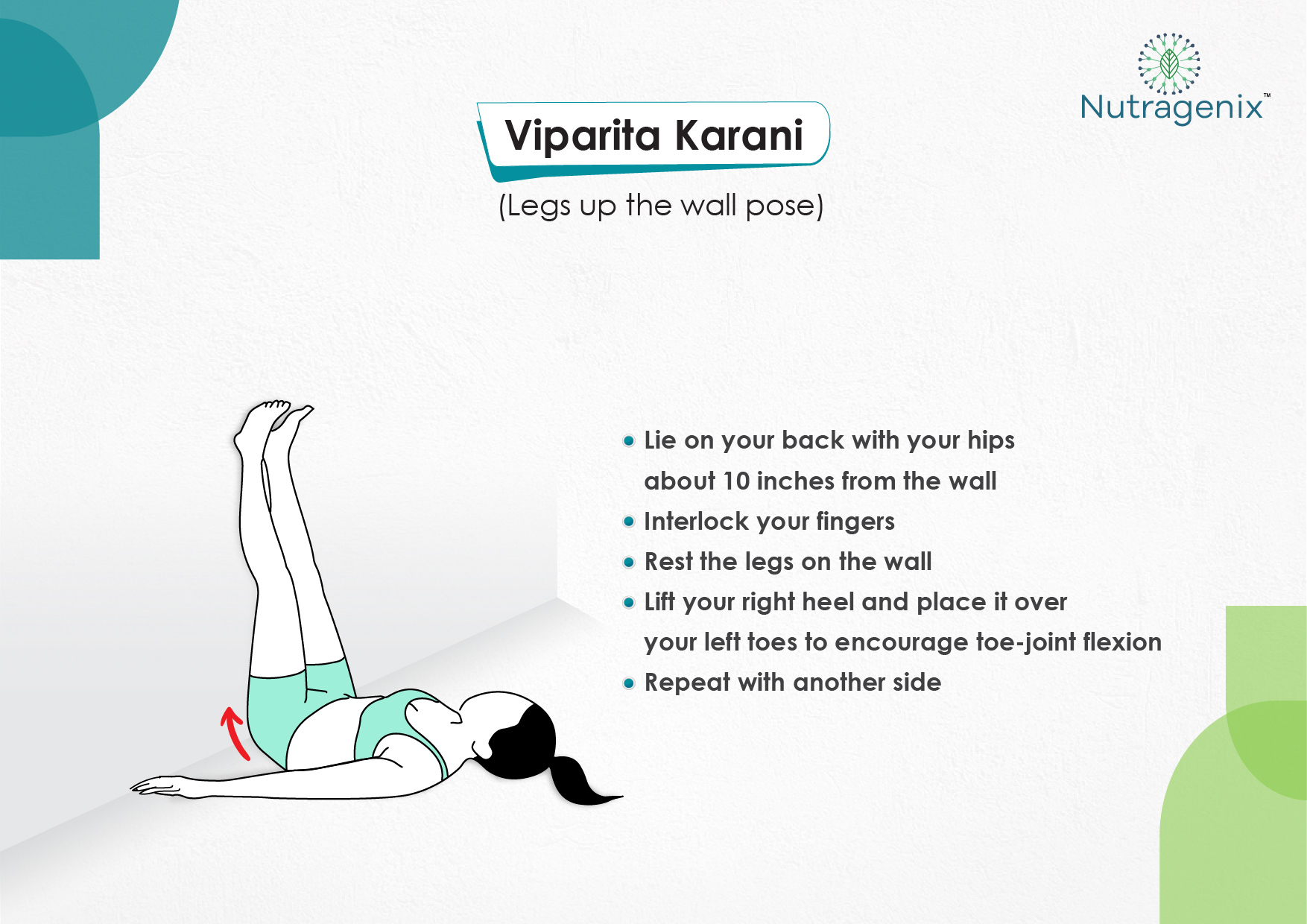
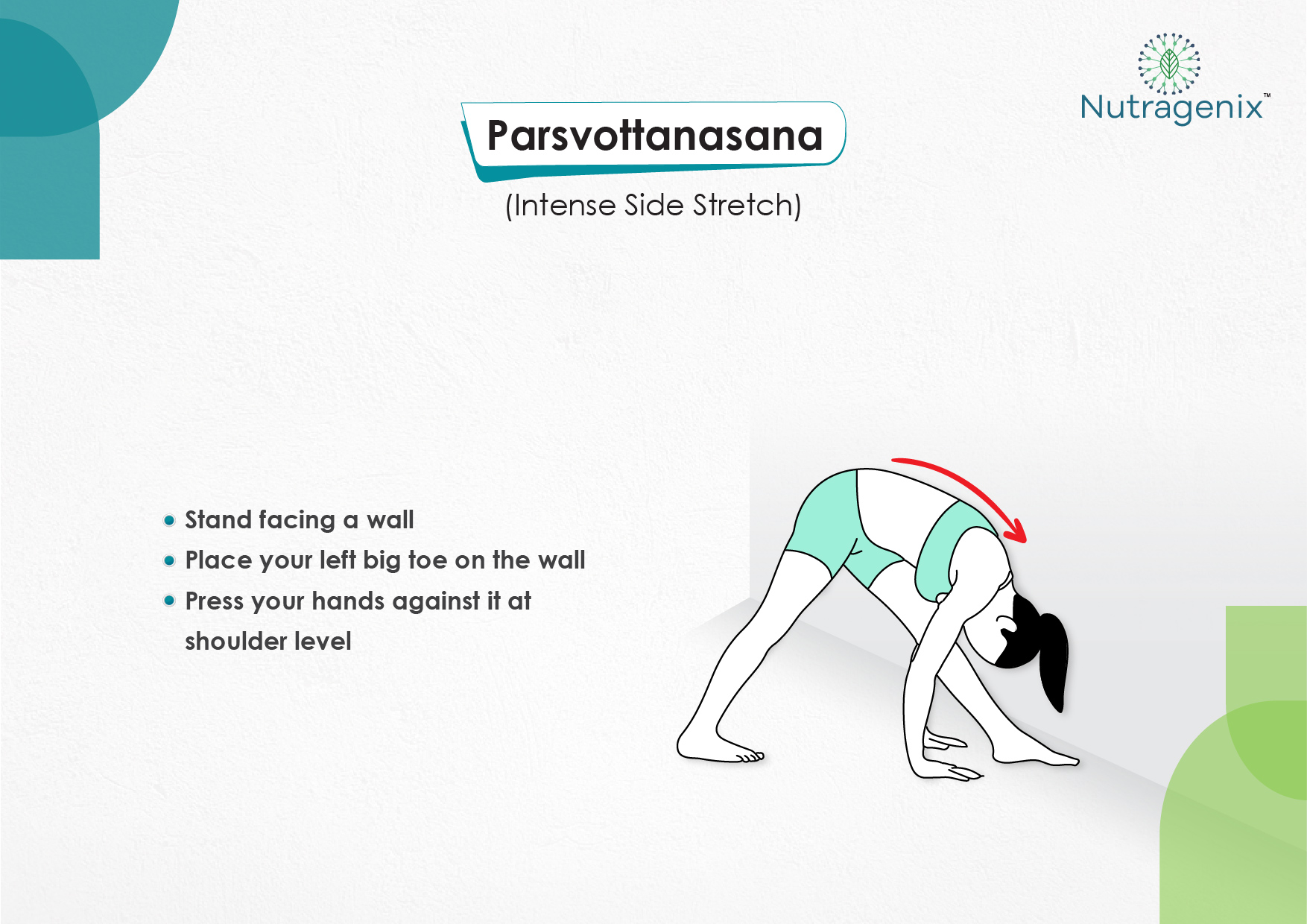
YOGA FOR OSTEOARTHRITIS
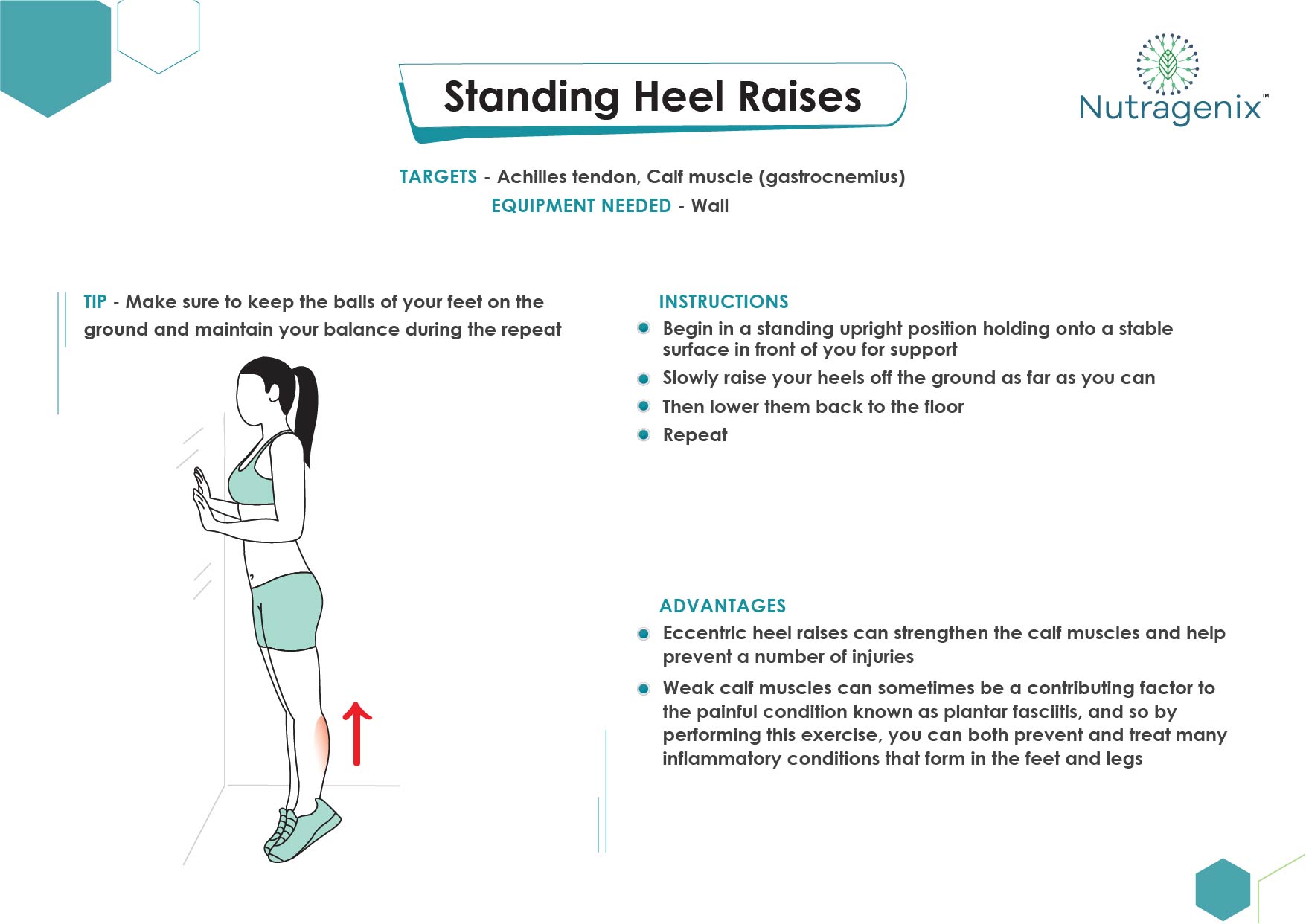
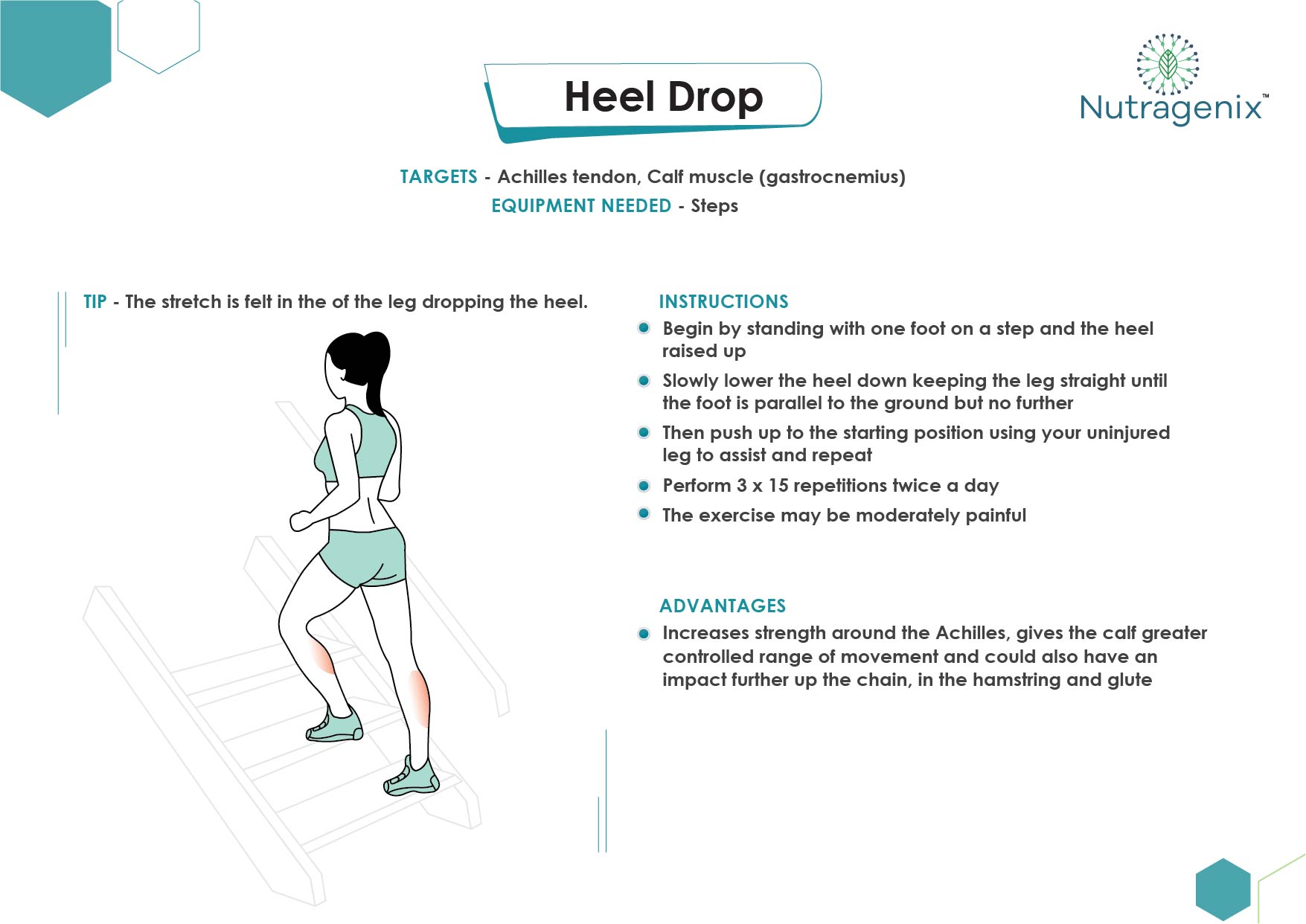
EXERCISES FOR TENDINOPATHY

NUTRACEUTICALS FOR OSTEOARTHRITIS
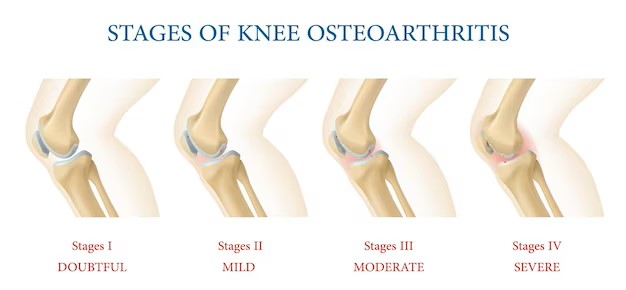
Knee osteoarthritis is a painful, chronic, degenerative disorder due to the progressive loss and wear and tear of the articular cartilage. The prevalence of osteoarthritis (OA) in India is about 28.7%, among which the majority are women.
Its treatment begins with symptomatic relief such as anti-inflammatory medications, painkillers and progresses to surgical treatment options. Recently, nutraceuticals derived from herbs are stealing attractions in the management of knee OA as it plays a vital role in slowing the destruction of joints and reduction of inflammation.
Few Nutraceuticals useful in the management of knee osteoarthritis are Curcumin, Fish Oil, Ginger, Green tea, Rosehip extract, Boswellia, Collagen peptide, Glycosaminoglycans.
The analgesic, anti-inflammatory, chondroprotective, and anti-arthritic actions of these nutraceuticals play a significant role in the management of knee OA. Nutraceutical supplements not only provide symptomatic relief but also interfere in the degeneration of articular joints and slow down the OA progression. Numerous clinical studies reveal that it can be used as an adjunct therapy for the management of knee OA because of its good safety and efficacy profiles.
Patient Education On Osteoarthitis
An Initiative by Nutragenix Healthcare Pvt. Ltd.